Massive change in the healthcare sector. With a looming worldwide recession in the wake of the COVID-19 pandemic, disruptive technological transformations, and the demand for value-based care across the industry, key stakeholders must anticipate and adapt in order to thrive in the dynamic new healthcare paradigm — or be left behind.
To shed light on what healthcare tech leaders should prioritize in the year to come, let’s explore five healthcare priorities that illuminate where healthcare is heading.
Make Way for AI
Artificial intelligence (AI) adoption in healthcare has been slow but momentum is building. A survey by health insurer Optum found that 85% of healthcare executives have an AI strategy, and almost half of executives surveyed now actively use the technology. With this level of awareness, expect a dramatic shift in how healthcare operates.
Why the sudden buzz about AI? It’s because AI technology and standards can alleviate an embattled healthcare sector that faces high labor shortages, inflationary costs, and supply chain issues. A few of AI’s far-reaching applications include: early diagnosis of chronic illness through predictive models, comprehensive processing of both structured and unstructured data, and helping works fight burnout.
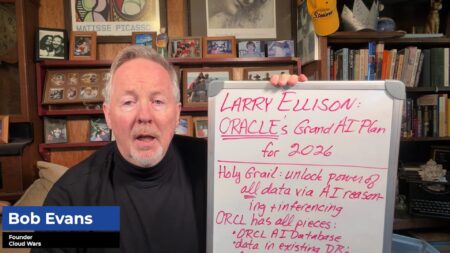
At Acceleration Economy’s Cloud Wars Expo held last summer, key AI industry players positioned themselves as prime movers to support AI use cases Dr. David Rhew, Microsoft’s Global Chief Medical Officer and Vice President of Healthcare, explained how the Dragon Ambient eXperience (DAX) uses AI to automatically generate clinical documentation of patient visits, which alleviates the administrative burden. He also explained how AI can be applied to telemedicine.
Oracle’s Nicholas Smith, Program Lead of Federal Digital Services, explained how cutting-edge AI and machine learning are now ready to process unstructured data due to the prevalence of cloud computing adoption.
Enhance Cybersecurity
Information security has become a major challenge for healthcare IT (HIT) teams in recent years due to the increase in remote access to company servers, personal devices in the workplace, and the demand for mobile access from physicians. This challenge is particularly pronounced for rural and critical access hospitals, which are often low on the list of potential applicants for cybersecurity professionals due to their remote operations and inability to offer competitive salaries. Due to these circumstances, IT staff who may not have the required tools or experience often have the responsibility of information security governance — and unfortunately these types of staffers make the perfect target for cybercrime.
Simultaneously, cybercrime is converging with advanced persistent threat methods, enabling cybercriminals to weaponize new technologies at scale to cause more disruption and destruction. This trend is expected to continue into 2023 and beyond, with the growing volume and variety of increasingly sophisticated cyber threats. Some of the new attack trends that are predicted to emerge are the explosive growth of crime-as-a-service (CaaS); the use of machine learning for money laundering and recruitment targeting; the increase in cybercrime in new online destinations such as virtual cities; and the proliferation of wiper malware.
To protect against these evolving threats, healthcare organizations are adopting a multi-layered security approach across all attack surfaces to protect themselves and their sensitive data, including:
- Endpoint protection
- Network security
- Cloud security
- Employee training and incident response plans
- Multi-factor authentication/password protection
- Security assessments
- Virtual Chief Information Security Officer services
Address The Looming Cost Issue
With healthcare bracing for soaring inflation, supply chain issues, and rising labor costs, addressing financial considerations is likely to top the list of healthcare priorities in 2023.
A recent McKinsey publication paints a dire picture of the situation:
- There will be a clinical labor shortage by 2025, with an expected gap of 200,000 to 450,000 registered nurses (10% to 20% of the workforce) and 50,000 to 80,000 doctors (6% to 10%)
- Incremental wage growth in the nonclinical workforce will potentially result in $90 billion in cost by 2027 throughout the entire healthcare system
- Ongoing supply chain difficulties and increased costs across the global economy are forecast to permanently push nonlabor costs by up to $110 billion in 2027
Other sources also point to the rising costs of drugs and medical supplies, further straining healthcare infrastructure.
With many hospitals already operating in the red, these sources are warning of service closures and potential systemic collapse without immediate outside support. This situation will force many governmental organizations to intervene to prevent catastrophe.
Reduce Health Inequities
Healthcare quality improvement has helped address inequities in care, but persistent health disparities remain, particularly among Black, Indigenous, and People of Color (BIPOC) populations. Some healthcare quality improvement initiatives have focused on data collection, analysis and evidence, as well as cost, payment, and financial rewards, and have been either provider-focused, payer-focused, or focused on both payers and providers.
One solution for reducing health inequities is focusing on social determinants of health (SDOH) in underserved communities. SDOHs consist of a myriad of factors, including safe housing and transportation, racism and discrimination, education and job opportunities, access to healthy food and physical activities, pollution, language and literacy skills.
SDOH contribute to health disparities and inequities, and addressing them is an important focus of Healthy People 2030, a national public health initiative in the United States. Healthy People 2030 includes many objectives related to SDOH, which are developed by subject matter experts in workgroups, including the Social Determinants of Health Workgroup.
Big Data is also playing a significant role in the reduction of health inequities in 2023. Researchers must focus on understanding the issues as well as improving insight into the social determinants of health and improving access to quality care for all populations. This can be achieved through the use of machine learning and precision medicine, as well as by improving data sharing and standards and increasing the representation of minorities and underserved populations in clinical trials. Similarly, telehealth can address these disparities by allowing patients to communicate with healthcare providers in their preferred language and providing culturally appropriate care.
Customer Segmentation
Healthcare companies are starting to adopt a more segmented approach to better address the needs of diverse populations. The segmented approach involves building bespoke insurance and care delivery models that are tailored to specific groups of people.
For example, Clever Care, a Medicare Advantage startup in Southern California, has grown significantly in the Asian community by offering specific benefits, building a carefully chosen network, and engaging with the community. Alignment Healthcare has introduced the “el Unico” option for the Hispanic population, and SCAN Health Plan has partnered with Included Health to launch the Affirm product for the LGBTQ+ community. These products provide differentiated services and benefits and also allow for growth that may not have been possible otherwise.
On the care delivery side, there are also a growing number of startups focusing on ethnic populations. Zocalo Health, founded by Amazon Care alumni, is a clinical company “by Latinos for Latinos.” The idea that all patients should receive the same clinical model is being challenged, which is a positive development.
It is unclear whether these offerings will be successful in the long term, but they are worth watching throughout 2023 as companies seek to align with diversity, equity, and inclusion initatives while also trying to drive results.
Final Thoughts
This is a time of transformation in the healthcare sector, with a focus on artificial intelligence, addressing rising costs, reducing health inequities, customer segmentation, and cybersecurity. At Acceleration Economy, we’ll continue to offer the latest on how healthcare stakeholders are adapting to these challenges in an evolving, turbulent, and exciting healthcare paradigm.
Want more tech insights for the top execs? Visit the Leadership channel: